Will A Bolus Of Hydromorphone Put Me To Sleep?
Annotation: This guideline is currently under review.
Introduction
Aim
Definition of Terms
Pharmacology
Cess
Management
Special circumstances
Companion documents
Links
Evidence Tabular array
Introduction
Opioid analgesia is indicated for the treatment of moderate to severe pain. An opioid is a medication that relieves pain by binding to opioid receptors in the central nervous arrangement spinal cord and peripheral nervous organisation. This guideline does not cover opioid delivery via patient controlled analgesia (PCA) commitment.
Aim
To provide medical and nursing staff at the Majestic Children's Hospital with a clear outline for assessment and management of a patient receiving opioids as an inpatient, including administration and agin events associated with assistants.
Definition of Terms
- Authorised persons: Nurse or medical staff registered to administrate opioids
- CPMS: Children's Pain Management Service (astute hurting)
- Elapsing of action: Fourth dimension the drug activity lasts at an constructive concentration
- Half-life: Time information technology takes for the medication to reduce by 50% in the plasma level
- Four: Intravenous
- Miosis: Excessive constriction of the pupil of the eye
- Myoclonus: Spasmodic jerky contraction of groups of muscles
- Opioid agonist: A medication with maximal physiological effect at the opioid receptors eastward.g. morphine
- Opioid antagonist: A medication that occupies the opioid receptors simply has no physiological action e.g. naloxone
- SC: Subcut
- Tremor: Involuntary contraction or twitching of one or more than body parts
- VPPCP: Victorian Paediatric Palliative Care Program
Pharmacology
There are three principal types of opioid receptors, these receptors accept multiple actions:
Mu (m) receptors are primarily responsible for analgesia and side effects of opioids and are associated with analgesia and side effects (Table 1). Side effects occur regardless of which opioid is used and are generally dose related. Mu receptors subtyped: mu-1 & mu-2
- mu-i receptor is primarily responsible for analgesia
- mu-ii receptor is primarily responsible for the opioid side effects
Delta (d) receptors are involved with modulation of mu receptors. Primarily responsible for spinal analgesia
Kappa (1000) receptors are associated with miosis, spinal analgesia and sedation
Opioids are metabolised in the liver and excreted via the kidneys. Morphine is the near commonly used opioid of choice, and has two main metabolites M3G and M6G. M3G (morphine -3 glucuronide) has no analgesic activeness, but tin cause neurotoxic effects such every bit tremor and myoclonus. M6G (morphine – half-dozen – glucuronide) is a powerful analgesic.
Table 1: Side effects of opioids
Neurological
- Sedation
- Euphoria
- Dysphoria
- Agitation
- Miosis
- Respiratory Depression
Cardiovascular
- Bradycardia
- Vasodilation
- Hypotension
- Pruritus (itch) *
Gastrointestinal/Renal
- Nausea & Vomiting
- Constipation
- Delayed gastric elimination
- Reduced appetite
- Urinary retentiveness
Musculoskeletal
- Muscle rigidity**
*Fentanyl primarily on the face, Morphine generalised
**Astute consequence of IV fentanyl
Table 2: List of opioid medications
| Opioid generic name | Medication information |
| Morphine |
|
| Fentanyl |
|
| Hydromorphone |
|
| Oxycodone |
|
| Tramadol |
|
Assessment
Regular observations (Table 3) of patients are indicated during the fourth dimension a patient receives an opioid infusion to monitor the efficacy of pain management. Pain assessment and measurement every bit per the clinical nursing guideline, and to recognise and forestall adverse effects such as sedation and respiratory depression. More frequent observations should be undertaken in patients receiving an administration of an opioid bolus. Patients receiving opioid infusions in the loftier risk category (Table three) are ideally admitted to a room that supports line of sight past nursing staff (e.g. close to the central desk in each pod). Patients in Tabular array 5 require continuous pulse oximetry while for the duration of their opioid infusion due to their high take chances of an adverse effect. Effectiveness of the analgesia and any bolus administration should be recorded in the patient's EMR progress notes
- Sedation nearly e'er precedes respiratory low, therefore this is the most important observation as a clinical indicator
- Any observations that transgresses the yellowish zone VICTOR nautical chart criteria should be reported to the treating squad and CPMS (observations that transgress ruby-red zone MET criteria should found a MET call 22 22)
- Infants 6 months or less who run into the criteria in Tabular array 6 should be monitored following any surgical procedure for the first 24 hours of opioid therapy in intensive care. These patients are at college risk due to the combination of opioid administration intraoperatively and postal service operatively, hurting and splinting, fluid overload and gamble of hypoventilation.
- Pain assessment and score to exist documented as per Table 3 and Table 4
Table 3: Observations required for documentation for a patient receiving an opioid infusion
- Pulse oximetry: hourly for duration of opioid infusion
- Sedation score, respiratory rate and heart rate:
1 hourly until the opioid infusion is ceased and then observations should be performed in conjunction with the Observation and Continuous Monitoring Guideline
- Pain score:
1 hourly while awake
- Airsickness score:
ane hourly for the first 12hrs, then 4 hourly every bit indicated
Table 4: Observations required for documentation for a patient following administration of a bolus
- Sedation score and Respiratory rate: every 5 minutes for 15 minutes and then render to routine observations.
- Pulse oximetry: if indicated and for all infants nether 6 months of age
- Pain assessment Pain score prior to and following the bolus
Table 5: Patients considered at loftier risk of an adverse event
- Infants 6 months or less
- Ex-premature infants
- Patients with a history of slumber apnoea or airway obstacle
- Airway surgery e.g. tonsillectomy and/or adenoidectomy
- Pre-existing respiratory co-morbidity e.g. recent RSV infection
- Patients with comorbidities including cerebral palsy, craniofacial disorders, muscular dystrophy or neurological conditions including neurosurgery or traumatic brain injury
- Concurrent employ of sedatives or mucopolysaccarides
- Renal impairment
Table half-dozen: Criteria for mail service-operative monitoring in intensive intendance
- Significant prematurity eastward.chiliad. <35 weeks at risk of apnoea
- History of apnoea
- Chronic lung disease
- Significant co-morbidities (eastward.g. airway abnormalities, cardiac abnormalities, significant caput trauma/neurological disease)
Who are undergoing a surgical procedure and are probable to require a narcotic infusion or oral opioid in the post-operative period, are at high risk for apnoea and deterioration on the wards. This can occur considering of the combination of amazement, opioid analgesia, pain and diaphragm splinting, fluid overload, and belatedly identification of under-ventilation. These infants should be monitored in PICU for the first 24 hours, then when stable returned to the ward. Monitor these infants with oximetry, respiratory rate monitoring, no oxygen unless hypoxaemic, and monitor analgesia requirements and fluid remainder.
Direction
Opioid infusion preparation
A continuous opioid infusion can provide continuous analgesia without the peaks and troughs of intermittent bolus only administration
- The opioid infusion must be prepared in accordance with RCH medication management policy and the syringe labelled clearly with a blue intravenous additives label.
- The infusion pump and infusion line should be clearly labelled with the small blue IV opioid infusion labels as an additional condom characteristic.
- The two authorised persons who brand up each opioid syringe must sign and verify the record of infusion
- Preparation and dilution of opioids every bit outlined in Table seven: Intravenous preparation of opioids for infusions.
- An infusion pump must exist used for all opioid infusions and programmed using the appropriate guardrails profile and medication.
- Bolus doses of opioid infusion (as prescribed on 'Opioid Infusion ') should ONLY be administered using the 'bolus button' on the syringe pump, which delivers the bolus in increments of up to 2 mL. If the syringe pump is in the 'ON' mode during the bolus, this volition add the bolus volume to the total volume infused. The hands costless fashion is preferable for delivering a bolus.
- Rosella and Butterfly intensive care units have special considerations in regards to preparation and administration.
Tabular array 7: Intravenous preparation of opioids for infusion
| Medication | Grooming | Infusion rate | Recommended bolus |
| Morphine | 0.5mg/kg in 50mL 0.9% saline or 5% dextrose | 0-4mLs/hr (0-40 micrograms/kg/hr) | Initial bolus 5mL (50mcg/kg) PRN For pain or painful procedures 1-2 mL (10-20mcg/kg) at intervals no less than 10 minutes |
| Fentanyl | 15 mcg/kg in 50mL 0.nine% saline or 5% dextrose | 0-4mLs/60 minutes (0-1.2 mcg/kg/hour) | Initial bolus 2mL (0.6mcg/kg) For hurting or painful procedures 1mL (0.3mcg/kg) at intervals no less than five minutes |
| Hydromorphone | 0.1mg/kg in 50mL 0.9% saline or 5% dextrose | 0-4mLs/60 minutes (0-8 mcg/kg/hr) | No initial bolus For pain or painful procedures one-2mL (ii-iv mcg/kg) at intervals no less than 10 minutes |
| Oxycodone | 0.5mg/kg in 50mL 0.9% saline or 5% dextrose | 0-4mLs/hr (0-40mcg/kg/hour) | Initial bolus 5mL (50mcg/kg) For pain or painful procedures 1-two mL (10-20mcg/kg) at intervals no less than ten minutes |
| Tramadol | 4mg/kg in 50mL 0.9% saline or five% dextrose | 0-4mLs/60 minutes (0-0.32 mg/kg/hr) | No initial bolus For pain or painful procedures 1-ii mL (0.08-0.16mg/kg) no less than 10 min |
Opioid infusion administration
- Unless the patient has received a recent dose of opioid, a loading dose should be administered (according to the Ballsy prescription) at the kickoff of the infusion to ensure therapeutic plasma levels are quickly reached.
- For rapid relief of pain (or anticipated pain), the prescribed bolus dose should be administered.
- The infusion rate may be adjusted by the nurse within the dose range specified, according to the patient's level of hurting.
- Information technology takes approximately iv one-half-lives (~8hrs for morphine/hydromorphone, ~1.5hrs for fentanyl) to reach steady state plasma concentration if given as an infusion, therefore if the charge per unit is to be increased, a bolus should be given likewise.
- Ideally the infusion charge per unit should not be increased unless 3 boluses are required in a 1 hour period.
- The volume infused should exist checked every hr and charge per unit verified on the fluid balance menstruation chart.
Adverse Effects
Patient receiving an opioid infusion may be at risk of adverse effects including pruritus, urinary retentivity, and respiratory depression or over sedation. The treatment of intolerable opioid side effects is the opioid antagonist naloxone. The half-life of Naloxone is 30-lx minutes, therefore if a patient is given Naloxone for sedation or respiratory depression they must exist monitored for four hours. Naloxone is available in the ward impress drug closet and on the ward resuscitation trolley.
Table viii: Naloxone doses for side effects
| Naloxone indication | Dose | Maximum dose per administration |
| Opioid induced pruritus and urinary retention | 1 microgram/kg | 100mcg |
| Excess sedation | ii microgram/kg | 200mcg |
| Resuscitation | x microgram/kg | 400mcg |
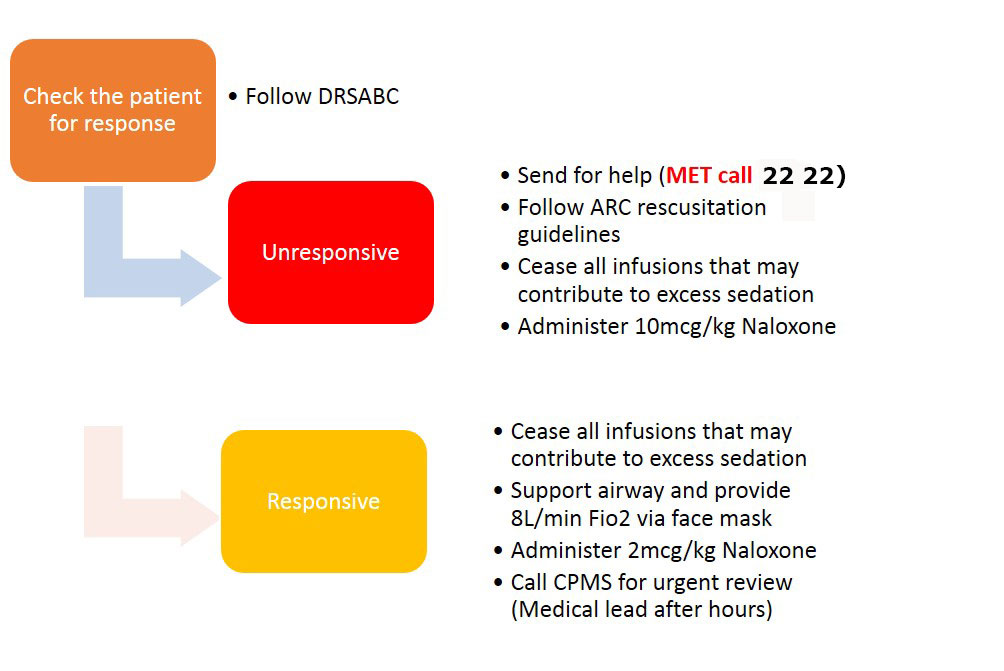
- Refer to Figure 1 for steps to follow in the upshot of respiratory low or over sedation
- Both M3G and M6G metabolites may accumulate in patients receiving long-term morphine infusions or patients with renal damage.
- Prolonged fentanyl infusion may event in drug accumulation and potential increment in opioid related side effects.
- Development of opioid tolerance with long-term assistants of opioids may require the opioid dose to be increased or an opioid rotation. Careful tapering of doses is important when weaning long-term opioids to avoid opioid withdrawal.
Figure 1: Response to over sedation or respiratory depression events
CPMS Review
- Non all patients receiving opioid infusions are under the supervision of CPMS. If the primary treating team wishes the patient to be seen by CPMS, a referral needs to be made by one of the treating team by paging 5773 (24 hours) and completing an electronic inpatient referral. The referrer needs to ensure that the patient's principal consultant has approved CPMS involvement.
- CPMS reviews patients twice daily on week days and once daily on weekends and public holidays.
- If analgesia is inadequate or the patient is experiencing side-effects, CPMS must be called to review the patient.
- CPMS can be contacted at all times on pager 5773 or ASCOM 52702
Ceasing an opioid infusion
- The determination to cease the opioid infusion should ideally be made in consultation with CPMS.
- Oral opioids may exist administered immediately afterwards the opioid infusion is ceased.
- Any remaining opioid infusion must be disposed of according to Drugs, Poisons and Controlled Substances Regulations (2006), Division 7.
Special Circumstances
Concurrent medications
- When opioid infusions are used, NO ADDITIONAL ORAL/ INTRAVENOUS opioids or allaying agents should be given without prior consultation with CPMS or an anaesthetist.
- Paracetamol, clonidine, ketamine, local anaesthetics, tramadol and NSAIDs, gabapentin may be prescribed and administered concurrently with opioid infusions. They may help to reduce opioid requirements and associated side effects.
- If the patient is receiving other medication that may cause sedation (e.g. antihistamines, benzodiazepines, baclofen pump or anticonvulsants), the patient may be at increased take a chance of sedation and respiratory depression.
Palliative care
- Regular monitoring such as blood pressure and temperature, pulse and respiratory rate are not as essential in palliative care patients- can be negotiated with ward staff and families. Please check the patient hourly.
- Hurting and symptom management is essential and must be carried out hourly including administration of site cheque.
- Doses are calculated on a 24 hr period rather than hourly infusions rates. Guidance will be provided by VPPCP. If there are concerns about opioid toxicity we strongly recommend assessment of pupils and the use of naloxone should be considered charily and in consultation with VPPCP given it may exacerbate a pain crunch during finish of life care.
- Infusions may be delivered subcutaneously rather than intravenously. Delight refer to the Subcutaneous catheter devices management CPG.
Butterfly
- Pain assessment is performed using the mPAT. The mPAT is a valid, reliable, clinically useful and viable tool. See: Neonatal Hurting Assessment CPG
- Preparation of opioids is of a different strength equally per unit policy, infusions should be changed prior to discharge from Butterfly to RCH inpatient wards
- The half-life of opioid analgesics may be increased and renal drug excretion may be prolonged due to immature renal function.
- Neonates on opioid analgesic medications should take continuous cardiorespiratory monitoring (ECG, RR, Sp02). The only exception for this would be on understanding with neonatal consultant when oral opioids are weaning and have reached minimal dosing.
- Patients receiving IV opioid boluses that are as well on continuous cardiorespiratory monitoring in the intensive care surround with ane:1 nursing are non required to document following the bolus as per Tabular array 4. However, if the patient becomes nursed in the special intendance nursery or as an HDU they must have observations following a bolus equally per Table 4.
Rosella
- Pain assessment is performed using the COMFORT B scale a validated tool for cess of pain in intubated and sedated children
- Preparation of opioids is of a dissimilar strength as per unit policy, infusions should exist changed to ward forcefulness prior to discharge from Rosella to RCH inpatient ward
- Intubated and ventilated patients are provided a larger bolus dose of opioid due to their protected airway and supported ventilation
- Nurses caring for patients in Rosella that require opioids should be familiar with the PICU pain and sedation guideline and protocol
- Patients receiving IV opioid boluses that are also on continuous cardiorespiratory monitoring in the intensive care environment with 1:1 nursing are not required to certificate following the bolus equally per Tabular array 4. Yet, if the patient becomes nursed as an HDU they must take observations following a bolus equally per Table iv.
ED
- Patients in ED are managed as per this guideline unless their destination is Rosella (PICU) or Butterfly (NICU) in which staff can prepare and manage the patient co-ordinate to that department'southward local guideline. This ensures the patient is adequately prepared for timely transfer from ED.
Companion Documents
- Pain assessment and management (basic) page 32 RCH Nursing competency framework, Chapter ii, Generic Competencies
- Pain (Analgesia Infusion) RCH Nursing competency framework, Affiliate 3, Cockatoo, Kelpie, Koala, Kookaburra, Possum, Rosella, Sugarglider
Links
- Pain assessment and management nursing guideline
- Neonatal Pain Assessment nursing guideline
- Ascertainment and Continuous Monitoring nursing guideline
- Medication management policy (RCH access merely)
- Drugs, Poisons and Controlled Substances Regulations (2006)
Prove Table
Evidence tabular array for the Management of the paediatric patient receiving opioids nursing guideline.
Please retrieve to read the disclaimer.
The development of this nursing guideline was coordinated past Grace Larson, CNC, Rosella, canonical past the Nursing Clinical Effectiveness Committee. Published Dec 2022.
Will A Bolus Of Hydromorphone Put Me To Sleep?,
Source: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Management_of_the_paediatric_patient_receiving_opioids/
Posted by: starkuplithim98.blogspot.com


0 Response to "Will A Bolus Of Hydromorphone Put Me To Sleep?"
Post a Comment